Understanding Pervasive Developmental Disorders
Pervasive Developmental Disorders (PDD) refer to a group of neurodevelopmental disorders that affect social interaction, communication skills, and behavior. These disorders typically manifest in early childhood and can have a significant impact on an individual’s daily functioning. Two key aspects of understanding PDD include an overview of PDD-NOS (Pervasive Developmental Disorder Not Otherwise Specified) and the relation of PDD to the autism spectrum.
Overview of PDD-NOS
PDD-NOS, which stands for Pervasive Developmental Disorder Not Otherwise Specified, was a subtype of autism that existed prior to the publication of the DSM-5 diagnostic manual in 2013. With the release of the DSM-5, individual subtypes of autism were consolidated into a single diagnosis known as Autism Spectrum Disorder (ASD). PDD-NOS encompassed individuals who displayed symptoms of autism but did not meet the criteria for a specific autism subtype.
PDD-NOS was characterized by delays in the development of socialization and communication skills, along with associated behaviors such as difficulties relating to people, delays in language usage, unusual play, resistance to changes in routine, and repetitive body movements or behavior patterns. Although PDD-NOS is no longer a separate diagnosis, individuals who previously received this diagnosis may now be diagnosed with ASD.
Relation to Autism Spectrum
Pervasive Developmental Disorders, including PDD-NOS, are now considered part of the broader category known as Autism Spectrum Disorder (ASD). ASD encompasses a range of neurodevelopmental conditions characterized by challenges in social interaction, communication, and behavior.
Within the autism spectrum, PDD-NOS represented a subtype that fell between the more severe Autism Disorder and the milder Asperger’s Syndrome. It included individuals with more severe autism symptoms than those with Asperger’s Syndrome but less severe symptoms than those with Autism Disorder. This reclassification under the umbrella term of ASD allows for better recognition and understanding of the diverse range of presentations within the spectrum.
It’s important to note that ASD is the most common subtype within the autism spectrum, accounting for approximately 47% of all ASD diagnoses. This highlights the significance of PDD-NOS and its inclusion as part of the broader autism spectrum.
Understanding the overview of PDD-NOS and its relation to the autism spectrum provides a foundation for comprehending the complexities of pervasive developmental disorders. By recognizing and acknowledging the various manifestations within the spectrum, it becomes possible to provide appropriate support and interventions for individuals with PDD.
Symptoms and Challenges
Pervasive Developmental Disorders (PDD) encompass a range of conditions that affect communication, social interaction, and behavior. Understanding the symptoms and challenges associated with these disorders is key to recognizing and supporting individuals with PDD.
Communication Difficulties
One of the primary symptoms of PDD is communication difficulties. These challenges can manifest in various ways, depending on the individual. Some individuals may have limited speech and struggle to express their thoughts and needs. Others may have relatively average language development but struggle with pragmatic language skills, such as understanding and using nonverbal cues and maintaining conversations. Additionally, individuals with PDD may exhibit repetitive or unusual speech patterns [4].
Social Interaction Challenges
Social interaction challenges are another hallmark of PDD. Individuals may have difficulty understanding social cues, such as facial expressions and body language, which can make it challenging to engage in reciprocal conversations and form meaningful relationships. They may struggle with taking turns, sharing interests, and demonstrating empathy. These difficulties can lead to social isolation and difficulties in forming and maintaining friendships [3].
Varying Severity Levels
The severity of symptoms and challenges associated with PDD can vary widely among individuals. PDD encompasses a spectrum, with some individuals experiencing more severe symptoms and impairments, while others may have milder manifestations. Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS) specifically falls within this spectrum, including children with more severe autism than Asperger’s syndrome but less severe than autistic disorder.
To better understand the variations in PDD, individuals diagnosed with PDD-NOS can be placed into different subgroups based on their strengths and challenges. This highlights the wide range of abilities and difficulties within the PDD-NOS population.
Recognizing the symptoms and challenges associated with PDD is crucial for early identification and intervention. By understanding the unique struggles individuals with PDD face in communication, social interactions, and varying severity levels, we can provide the necessary support and resources to help them thrive.
Causes and Risk Factors
To understand the causes of pervasive developmental disorders (PDD), researchers are exploring various factors, including genetic components and environmental influences. While the exact cause of PDD is still being investigated, it is believed that a combination of genetic and environmental factors contributes to the development of these disorders.
Genetic Components
Genetics plays a significant role in the risk of developing pervasive developmental disorders. Although there is no single “autism gene” identified as the sole cause of these disorders, research suggests that certain genetic conditions and family history of developmental disorders increase the risk of PDD [3].
While genetics are considered a risk factor, it’s important to note that there is no single gene responsible for these disorders. Ongoing research aims to unravel the complex genetic interactions and variations that contribute to the development of PDD.
Environmental Influences
In addition to genetic factors, environmental influences also play a role in the development of pervasive developmental disorders. Various prenatal and perinatal factors can increase the risk of PDD. Risk factors include advanced parental age, prematurity, low birth weight, and other factors that occur during pregnancy and childbirth.
It is essential to note that the relationship between genetics and environmental factors is complex. While certain genetic predispositions may increase susceptibility to environmental influences, the interplay between genes and the environment is still being studied.
Understanding the causes and risk factors associated with PDD is crucial for early detection and intervention. Identifying these factors can assist healthcare professionals in providing appropriate support and guidance for individuals with PDD and their families. Ongoing research in the field of genetics and environmental influences continues to shed light on the complex nature of pervasive developmental disorders.
Diagnosis and Early Intervention
When it comes to pervasive developmental disorders (PDD), early diagnosis and intervention play a critical role in supporting individuals with these conditions. In this section, we will explore the process of observational diagnosis and highlight the importance of early detection.
Observational Diagnosis
Diagnosing pervasive developmental disorders, including PDD-NOS (pervasive developmental disorder-not otherwise specified), primarily relies on observations of the child’s behaviors and information provided by parents or guardians. Unlike some medical conditions, there is no laboratory test available for diagnosing PDD. Healthcare professionals carefully assess various aspects of a child’s development, including communication skills, social interactions, and behavioral patterns.
During the diagnostic process, doctors may use standardized assessments and questionnaires to gather information about the child’s behaviors and development. These may include assessments such as the Autism Diagnostic Observation Schedule (ADOS) or the Childhood Autism Rating Scale (CARS). Through these observations and assessments, healthcare professionals can evaluate the child’s symptoms and determine whether they meet the criteria for a PDD diagnosis.
Importance of Early Detection
Early detection of pervasive developmental disorders is crucial for several reasons. Firstly, it allows for timely access to appropriate resources and interventions that can help children with PDD reach their full potential [5]. Early intervention can provide essential support in areas such as communication, social skills, and behavior management.
Additionally, early diagnosis helps families and caregivers better understand the child’s needs and implement strategies to support their development. By identifying PDD early on, parents and caregivers can start building a network of professionals, therapists, and educators who specialize in working with individuals with PDD. This collaborative approach ensures that the child receives comprehensive care tailored to their unique needs.
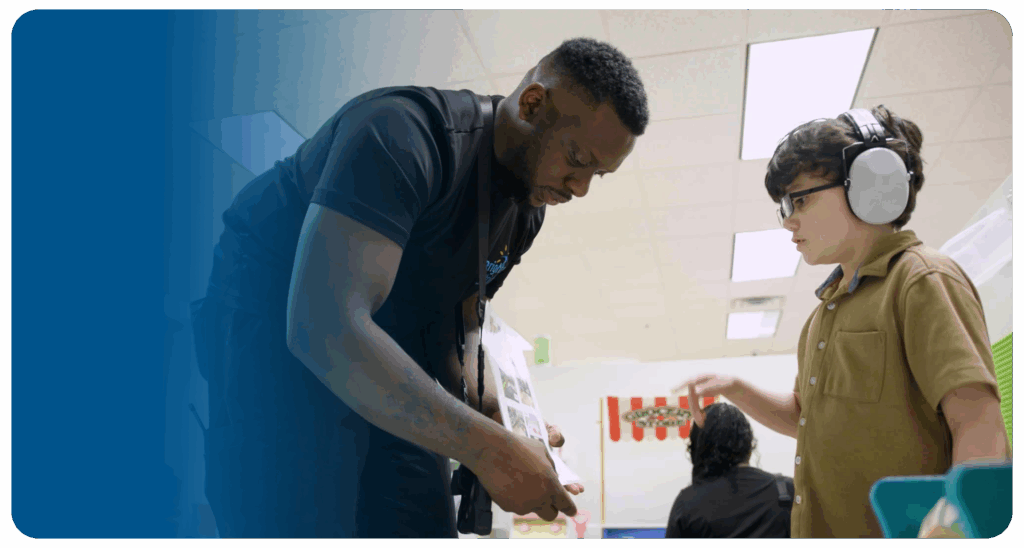
Moreover, early detection allows for the implementation of strategies to support the child’s educational journey. With an early PDD diagnosis, educational plans and accommodations can be put in place to facilitate learning and inclusion. Early intervention services, such as speech therapy, occupational therapy, and Applied Behavior Analysis (ABA), can be initiated to target specific areas of development and enhance the child’s overall progress [1].
In summary, early diagnosis and intervention are crucial for optimizing outcomes for individuals with pervasive developmental disorders. Prompt identification of PDD enables access to appropriate interventions, resources, and support systems. It empowers families and caregivers to provide the necessary tools for the child’s development, leading to better long-term outcomes and an improved quality of life.
Treatment Approaches
When it comes to treating pervasive developmental disorders (PDD), a comprehensive approach is essential. The treatment focuses on addressing the core symptoms and challenges associated with PDD, such as communication difficulties, social interaction challenges, and varying severity levels. While there is no known cure for PDD, various treatment approaches can help individuals with PDD lead fulfilling lives.
Therapeutic Interventions
Therapeutic interventions play a crucial role in the treatment of PDD. These interventions are tailored to the specific needs of each individual and aim to promote improved social and communication skills while minimizing the effect of behavioral problems that may interfere with learning and functioning [6]. Some commonly used therapeutic interventions include:
- Applied Behavior Analysis (ABA): ABA is a widely recognized and evidence-based intervention that focuses on reinforcing positive behaviors and teaching new skills through structured and systematic behavior modification techniques. It helps individuals with PDD acquire and strengthen social, communication, and behavioral skills.
- Speech Therapy: Speech therapy is often a key component of treatment for PDD. It focuses on improving communication skills, such as expressive and receptive language abilities, speech articulation, and pragmatic language skills. Speech therapists use various techniques tailored to the individual’s needs to enhance their communication capabilities.
- Occupational Therapy (OT): OT aims to improve an individual’s fine motor skills, sensory integration, self-care abilities, and overall independence. Occupational therapists work with individuals with PDD to develop strategies and provide support for daily living tasks, sensory processing challenges, and motor skill development.
- Social Skills Training: Social skills training helps individuals with PDD develop appropriate social interactions, understand social cues, and navigate social situations. It involves teaching social rules, perspective-taking, and problem-solving strategies to enhance social communication and relationships.
Medications and Complementary Methods
Medications may be used to address specific behavioral problems associated with PDD. However, it’s important to note that there is no specific medication to treat PDD itself. The use of medications is typically based on the individual’s specific needs and may vary from person to person. Medications are prescribed to manage symptoms such as aggression, hyperactivity, anxiety, or mood disturbances.
Complementary methods can also be used alongside therapeutic interventions and medications to support individuals with PDD. These methods may include:
- Alternative and Augmentative Communication (AAC): AAC systems, such as visual supports, picture schedules, and communication boards, can assist individuals with PDD in expressing their needs, wants, and thoughts when verbal communication is challenging.
- Sensory Integration Therapy: Sensory integration therapy helps individuals with PDD manage sensory processing challenges. It involves activities that address sensory sensitivities and help individuals regulate their responses to sensory stimuli.
- Dietary and Nutritional Approaches: Some individuals with PDD may benefit from dietary modifications or nutritional supplements. However, it’s important to consult with a healthcare professional or registered dietitian before implementing any dietary changes.
- Parental and Family Support: Providing support and education to parents and family members is an integral part of the treatment process. Parent training programs and support groups can help families navigate the challenges of raising a child with PDD and learn effective strategies for managing behaviors and promoting development.
By utilizing a combination of therapeutic interventions, medications when necessary, and complementary methods, individuals with PDD can receive comprehensive support to improve their quality of life and enhance their overall functioning. Treatment for PDD is individualized and should be tailored to address each person’s unique strengths, challenges, and needs.
Living with Pervasive Developmental Disorders
Living with a pervasive developmental disorder (PDD) can present unique challenges and require specialized support. In this section, we will explore two important aspects of living with PDD: educational support and enhancing quality of life.
Educational Support
Children with PDD may benefit from a variety of educational settings, depending on their individual needs and abilities. Some children thrive in specialized classrooms specifically designed for individuals with PDD, while others may excel in standard special education classes or even regular classes with additional support [4].
The goal of educational support for individuals with PDD is to provide an environment that promotes their academic, social, and emotional growth. This may include individualized education plans (IEPs) that outline specific goals, accommodations, and support services tailored to the unique needs of each child. These IEPs often involve a multidisciplinary team of professionals, including teachers, therapists, and support staff, working collaboratively to create a nurturing and inclusive learning environment.
It is essential for parents or caregivers to actively participate in their child’s educational journey. This involvement may include attending meetings, advocating for appropriate services, and maintaining open communication with teachers and other school staff. By working together, parents, educators, and professionals can ensure that children with PDD receive the necessary educational support to reach their full potential.
Enhancing Quality of Life
Enhancing the quality of life for individuals with PDD involves addressing various aspects of their well-being, including social, emotional, and physical needs. It is important to create an environment that fosters inclusion, acceptance, and understanding.
Supporting social interactions is crucial for individuals with PDD. Encouraging participation in social activities, such as clubs, groups, or community programs, can help develop social skills and build meaningful connections. Additionally, providing opportunities for individuals with PDD to engage in hobbies, sports, and creative outlets can contribute to their overall well-being and self-expression.
Promoting emotional well-being is equally important. This can involve the implementation of strategies to manage stress and anxiety, such as relaxation techniques or mindfulness practices. Creating a structured routine and providing clear expectations can also help individuals with PDD feel more secure and reduce feelings of uncertainty or frustration.
Furthermore, maintaining a healthy lifestyle, including proper nutrition and regular exercise, can positively impact overall well-being. Encouraging physical activities that align with the individual’s interests and abilities can contribute to their physical health and enhance their quality of life.
By implementing educational support tailored to the needs of individuals with PDD and focusing on enhancing their quality of life, it is possible to create a supportive and nurturing environment that allows them to flourish. It is vital to recognize that each person with PDD is unique, and their journey may require individualized approaches to best meet their specific needs and aspirations.
References
- https://www.autismspeaks.org/pervasive-developmental-disorder-pdd-nos
- https://www.webmd.com/brain/autism/autism-spectrum-disorders
- https://my.clevelandclinic.org/health/diseases/pervasive-developmental-disorders
- https://www.ninds.nih.gov/health-information/disorders/pervasive-developmental-disorders
- https://www.webmd.com/brain/autism/development-disorder
- https://www.asdclinic.co.uk/conditions/pervasive-developmental-disorder/how-are-pervasive-developmental-disorders-treated.php